As you may know, the Standards of Practice set out the minimum standards in paramedic services. Each regulated member is required to understand and comply with these Standards, but how does this translate in the day-to-day work of EMRs, PCPs and ACPs?
In an effort to help regulated members understand and apply the Standards to real life situations, we will be sharing scenarios that give context to the Standards and ideas on how to implement this into practice.
The following scenario will attempt to address patient health record access and content.
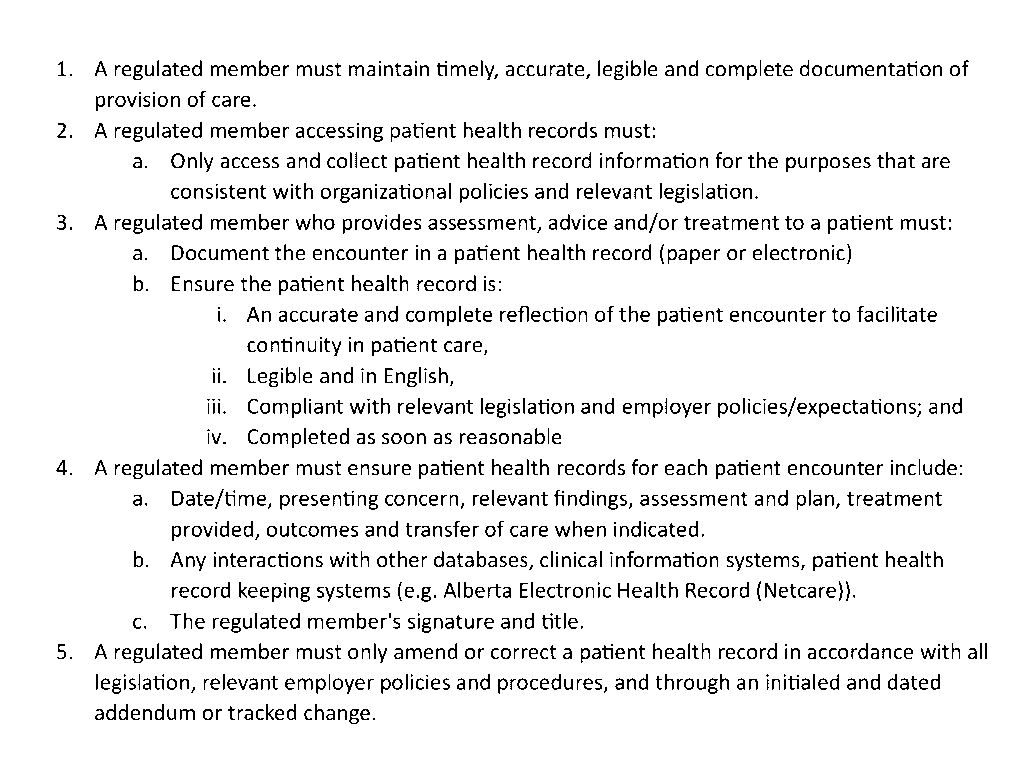
3.1 Patient Health Record Access and Content
Patient health records provide key information to other healthcare providers about assessments and interventions provided by a regulated member prior to transferring care of a patient. These records are critical in ensuring appropriate, timely continuity of care and preventing and minimizing adverse events.
Scenario:
Hadley, an Advanced Care Paramedic, is working as a Community Paramedic in Peace River. As part of her role, she provides scheduled in-home assessments and chronic condition support for patients referred through her place of employment. Because community paramedicine involves ongoing, collaborative care with family physicians, home care nurses and specialists, maintaining accurate and complete patient health records is essential for safe continuity of care.
On a morning visit, Hadley attends the home of Mrs. Desrochers, a 78-year-old patient recently discharged from the hospital after an exacerbation of congestive heart failure. Her referral outlines the need for assessment, Chem 8 lab work via iStat, medication reconciliation and patient education about fluid restriction.
During the visit, Hadley:
- Reviews the patient’s discharge medication list
- Takes vital signs and performs a focused assessment
- Identifies increased shortness of breath on exertion
- Notes mild pitting edema
- Reviews recent prescriptions, labs and echocardiogram findings in Netcare and Connect Care to contextualize the current symptoms
- Contacts the patient’s family physician by recorded phone call to request guidance on diuretic adjustments
After leaving the home, Hadley begins documenting the encounter in her patient care record. As she works through the record, she realizes that:
- She has not yet documented her review of Netcare prescriptions
- She did not include the specifics of the medication changes made at discharge
- She has not entered the details of her communication with the family physician
Under Standard 3.1: Patient Health Record Access and Content, Hadley recognizes that she is required to:
- Ensure the record is timely, accurate, legible and complete
- Document all assessments, findings, interventions, advice and communications
- Include all interactions with patient health information systems, such as Connect Care and Netcare
- Access health information only for authorized clinical purposes
- Complete the record as soon as reasonable
Hadley immediately updates the patient care record, entering:
- Date/time, presenting concern, assessment findings and plan
- The medication reconciliation, including dosages
- The phone call with the family physician and the guidance received
- Her access to Netcare and the lab/diagnostic information reviewed
- Her signature and professional designation
Hadley completes the documentation promptly, ensuring it reflects the encounter accurately and supports the ongoing care that Mrs. Desrochers will receive from her broader healthcare team.
As a paramedic working in Alberta, Hadley understands that her employer is the custodian of health information, while she is considered an affiliate under the Health Information Act (HIA). This means Hadley must collect, use and disclose health information only as authorized, follow all custodian policies and protect patient information at all times.
This scenario demonstrates the Community Paramedic’s responsibility under Standard 3.1: Patient Health Record Access and Content, ensuring that each patient encounter is properly documented to support safe, coordinated care in the community.